Mystery of Sudden Cardiac Death: A Case of Left Ventricular Non-Compaction
Rohan Tripathi, BS, Farzana Hoque
1 Saint Louis University School of Medicine, St. Louis, Missouri
2 Associate Professor of Medicine, Department of Internal Medicine, Saint Louis University School of Medicine, St.Louis, Missouri
Left ventricular non-compaction is a rare myocardial disorder characterized by prominent left ventricular trabeculae and deep intertrabecular recesses. While most cases are asymptomatic, it presents within a wide spectrumof clinical manifestations including left ventricular dysfunction, ventricular arrythmias, systemic embolization, and sudden cardiac death. Diagnosis is made through imaging studies such as echocardiography and cardiac magnetic resonance imaging. We describe a case of asymptomatic left ventricular non-compaction detected in a patient with no clinical clues outside of a positive family history of sudden cardiac death.
Keyword: Left ventricular noncompaction Cardiomyopathy Trabeculations Cardiac MRI Cardiac CT Suddencardiacdeath
Mystery of Sudden Cardiac Death: A Case of Left Ventricular Non-Compaction
Rohan Tripathi, BS, Farzana Hoque
1 Saint Louis University School of Medicine, St. Louis, Missouri
2 Associate Professor of Medicine, Department of Internal Medicine, Saint Louis University School of Medicine, St.Louis, Missouri
Background
Left ventricular non-compaction (LVNC) is a rare myocardial disorder characterized by prominent left ventricular trabeculae and deep intertrabecular recesses. The annual incidence has been reported to be between 0.014% and 0.26%.1 The prevalence increases amongst patients with a positive family history and about 15% to 20% of cases are estimated to be inherited. While there are several genes associated with LVNC, the mutations are most located within MYH7, MYBPC3, and titin (TTN). Pathogenesis of the increased left ventricular trabecular tissue is thought to derive from two distinct mechanisms. The first of which suggests that genetic mutations result in overdeveloped trabeculated layer in the myocardium. The other process proposes that conditions that cause increased preload, such as hemoglobinopathies, cause increased trabeculations of the left ventricle. LVNC is often asymptomatic but can possibly present with left ventricular dysfunction, ventricular arrythmias, systemic embolization, and sudden cardiac death (SCD). These clinical manifestations are suspected to arise from microischemia paired with wall motion abnormalities leading to dilation and eventually failure of myocardium1. Diagnosis is mainly made through imaging studies such as transthoracic echocardiography (TTE) and cardiac magnetic resonance (CMR) demonstrating increased ratios of non-compacted to compacted myocardium2,3,4 Management primarily focuses on treatment of the clinical sequala.
Objective
We hope to shed some light on varying clinical manifestations of left ventricular non-compaction and how this can result in diagnostic challenges especially in asymptomatic cases such as this one. In addition, our case report also demonstrates the importance of detailed family history in the process of creating a diagnosis.
Case Report
A 65-year-old male with a past medical history of hypercholesterolemia was referred to a cardiologist to rule out malignant cardiovascular disease. His hypercholesterolemia is well controlled on a low dose statin and he leads a moderately healthy lifestyle, routinely running on the treadmill and lifting weights. The patient denies any chest pain, shortness of breath, palpitations or syncope. In addition, he is a non-smoker and does not heavily consume alcohol.Vitals were significant for blood pressure of 152/89.
There were no abnormal findings on physical examination and the patient displayed regular rate and rhythm with no murmurs on auscultation. However, the patient’s family history revealed that his brother passed away from sudden cardiac death at the age of 54 despite living a similarly healthy lifestyle and having no significant past medical history. The autopsy report demonstrated mild left ventricular hypertrophy with no pathogenesis in his coronary arteries, myocardium, nor pulmonary arteries. The echocardiogram for the patient showed normal left ventricular systolic function and end- diastolic function. The echo also showed the presence of a 2-layered structure and ratio of thick noncompacted layer to thin compacted ≥ 2, diagnostic of left ventricular non-compaction. Subsequent cardiac magnetic resonance imaging (MRI) revealed non-compacted to compacted ratio greater than 2.3 at end-diastole within the left ventricle is diagnostic of left ventricular noncompaction. Given these findings, an implantable cardioverter defibrillator was placed, and the patient was started on ramipril 10 mg daily for his hypertension. Subsequent echocardiograms redemonstrated previous findings and the patient continues to deny cardiac symptoms in the following years.
Discussion
Echocardiography is the preferred method for diagnosing left ventricular non-compaction (LVNC) and family screening. The two-dimensional echocardiography (2DE) is the most widely used diagnostic tool.2 While 2DE provides excellent visualization of the left ventricular cavity, it may not adequately assess the myocardium and endocardium throughout the left ventricle.The prominent trabeculations characteristic of LVNC can curve into the cavity, challenging the planar cuts of 2DE.
This can lead to misinterpretation of trabeculationsas"false tendons" or underestimation of LVNC severity.2 Multiple 2DE studies are often needed to diagnose LVNC due to its inherent limitations. In our case, diagnosis of the asymptomatic LVNC was made possible through the positive family history of SCD in the brother of the patient. This patient had no other clinical indication that would have led to obtaining the imaging studies necessary for diagnosis. While diagnosis of LVNC in general remains a challenge as most cases are asymptomatic, the most common clinical clues in symptomatic patients are related to heart failure.3,4,5 As our patient had a normal ejection fraction, they have been following current guidelines to obtain an echocardiogram every 3 years to assess for any further anatomic changes.3 Furthermore, if genetic testing had been pursued and demonstrated a known mutation, first degree relatives should also be tested.6 The prognosis of LVNC is dependent on the presence of clinical sequalae and management is conducted accordingly. For example, anticoagulation therapy is recommended for ejection fraction less than forty percent and the presence of arrhythmias such as atrial fibrillation.7,8 For LVNC patients with congestive heart failure, goal-directed medical therapy is advised.5 Implantable Cardioverter Defibrillator (ICD) placement is recommended for LVNC patients with ejection fraction less than thirty-five percent and severe ventricular tachyarrhythmias.5,9 Our patient had prophylactically received an ICD despite normal ejection fraction given the family history of SCD suspected to arise from a ventricular arrhythmia. Further future management for our patient should consist of a detailed neurological examination. A single-center prospective study demonstrated that 61% of LVNC patients also had a form of neuromuscular disease. Identification and management of possible comorbid muscular dystrophies can improve patient outcomes given their association with deterioration of left ventricular function and increased morality.10
.png)
Figure 1: Cardiac MRI showing non-compacted to compacted ratio greater than 2.3 at end-diastole within the left ventricle is diagnosticofleft ventricular noncompaction.
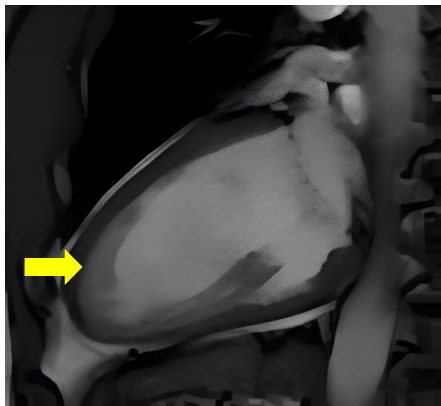
Figure 2: Cardiac MRI showing thickened trabeculae, reaffirming diagnosis of left ventricular noncompaction.
1. Singh DP, Horenstein MS, Rout P, et al. Left Ventricular Noncompaction Cardiomyopathy. [Updated 2024 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537025/
2. Song ZZ. Echocardiography in the diagnosis left ventricular noncompaction. Cardiovasc Ultrasound. 2008;6:64. Published 2008 Dec 23. doi:10.1186/1476- 7120-6-64
3. Sarma RJ, Chana A, Elkayam U. Left ventricular noncompaction. Prog Cardiovasc Dis. 2010 Jan- Feb;52(4):264-73. [PubMed]
4. Petersen SE, Jensen B, Aung N, Friedrich MG, McMahon CJ, Mohiddin SA, Pignatelli RH, Ricci F, Anderson RH, Bluemke DA. Excessive Trabeculation of the Left Ventricle: JACC: Cardiovascular Imaging Expert Panel Paper. JACC Cardiovasc Imaging. 2023 Mar;16(3):408-425. [PMC free article] [PubMed]
5. Shemisa K, Li J, Tam M, Barcena J. Left ventricular noncompaction cardiomyopathy. Cardiovasc Diagn Ther. 2013 Sep;3(3):170-5. [PMC free article] [PubMed]
6. Watts PJ, Garbo OS, Barrett W, Kopstein M, Maybrook R, Scherbak D. Flash Pulmonary Edema: A Case and Review of Left Ventricular Non-Compaction Cardiomyopathy. HCA Healthc J Med. 2020;1(4):205- 209. [PMC free article] [PubMed]
7. Chimenti C, Lavalle C, Magnocavallo M, Alfarano M, Mariani MV, Bernardini F, Della Rocca DG, Galardo G,Severino P, Di Lullo L, Miraldi F, Fedele F, Frustaci A. A proposed strategy for anticoagulation therapy in noncompaction cardiomyopathy. ESCHeart Fail. 2022Feb;9(1):241-250. [PMC free article] [PubMed]
8. Filho DCS, do Rêgo Aquino PL, de SouzaSilvaG,Fabro CB. Left Ventricular Noncompaction: New Insightsinto a Poorly Understood Disease. Curr Cardiol Rev. 2021;17(2):209-216. [PMC free article] [PubMed]
9. Klenda J, Boppana LKT, Vindhyal MR. Heart Failure Secondary to Left Ventricular Non-compaction Cardiomyopathy in a 26-Year-Old Male. Cureus. 2018Jul20;10(7):e3011. [PMC free article] [PubMed]
10. Stöllberger C, Blazek G, Gessner M, Bichler K,Wegner C, Finsterer J. Neuromuscular comorbidity, heart failure, and atrial fibrillation as prognostic factors in left ventricular hypertrabeculation/noncompaction. Herz. 2015Sep;40(6):906-11. [PubMed]